Cf. Allergies, urticaire, Oedème de Quincke
A intégrer: https://www.urgencesdirectinfo.com/dossier-mois/dossier-thematique-octobre-2017-anaphylaxie/10
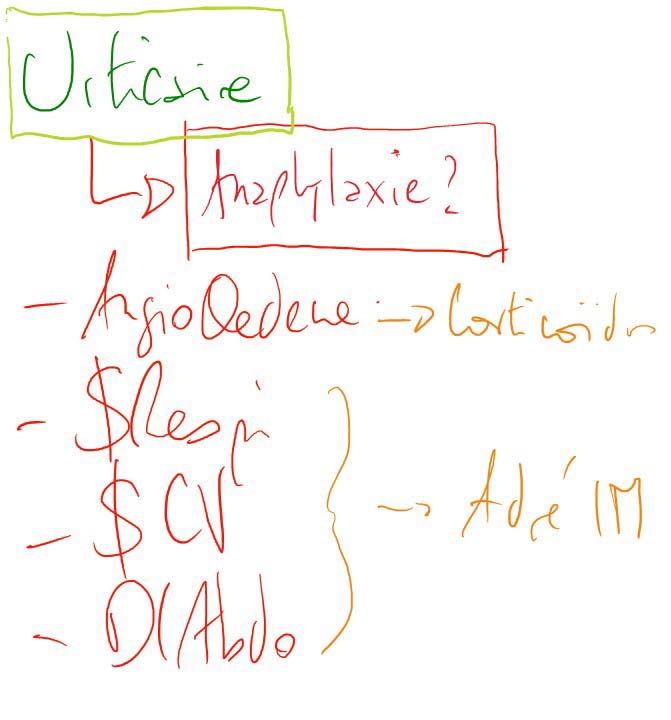
2 urgences:
Anaphylaxis is a clinical diagnosis.
Un trigger présent à 80% (15 à 30mn apres un lait, cacahouettes, coques chez l'enfant)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) recently issued new guidelines, which define anaphylaxis as:
In practice, anaphylaxis in the UK (and also Australia) is characterised by the presence of ‘Airway/Breathing/ Circulation’ (respiratory or cardiovascular) symptoms as part of an allergic reaction. Skin or mucosal changes alone are not a sign of an anaphylactic reaction.patients over 16 years are observed for 6–12 hours after anaphylaxis (children under 16 should be admitted).
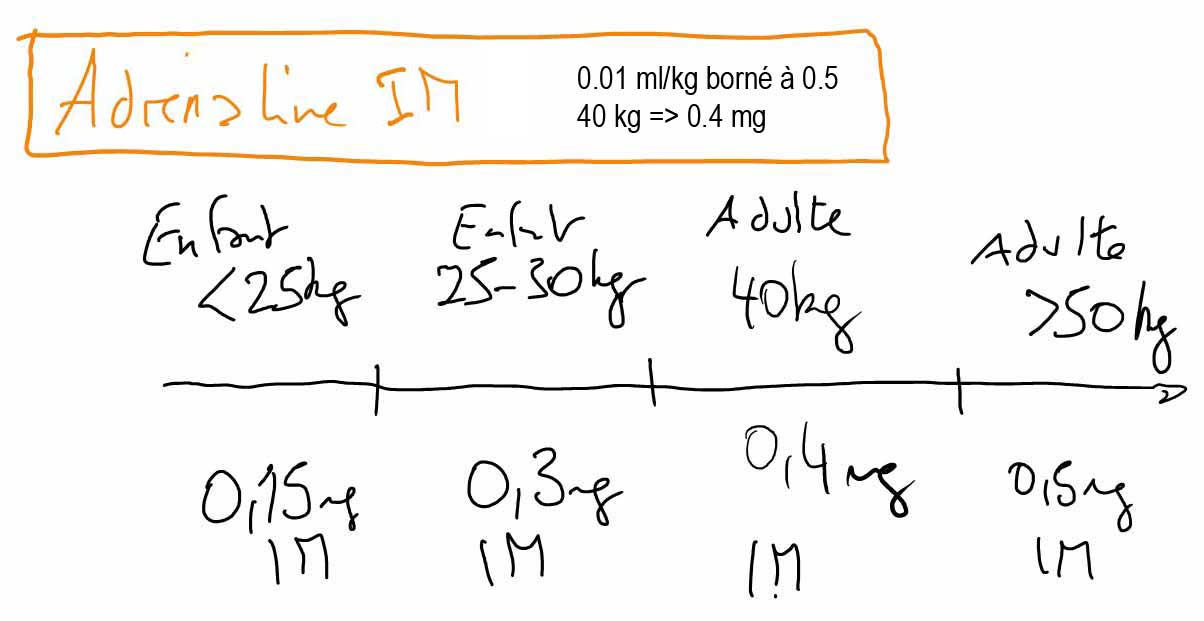
Le diagnostic d’anaphylaxie est clinique et repose sur l’utilisation des critères cliniques de Sampson:
La brutalité de l'installation est un critère de gravité. [RFE anaphylaxie SFMU 2016]
(ou Oedème de Quincke)
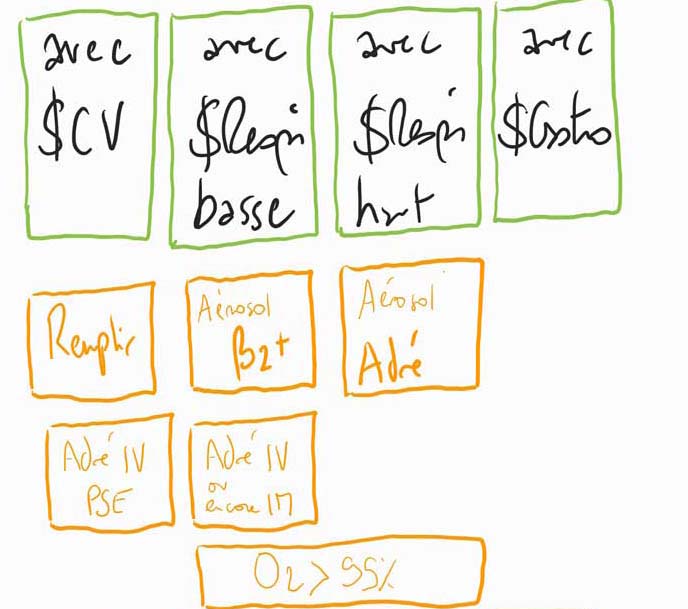
Si choc net: Adrénaline IV ? ou bien on commence par IM?
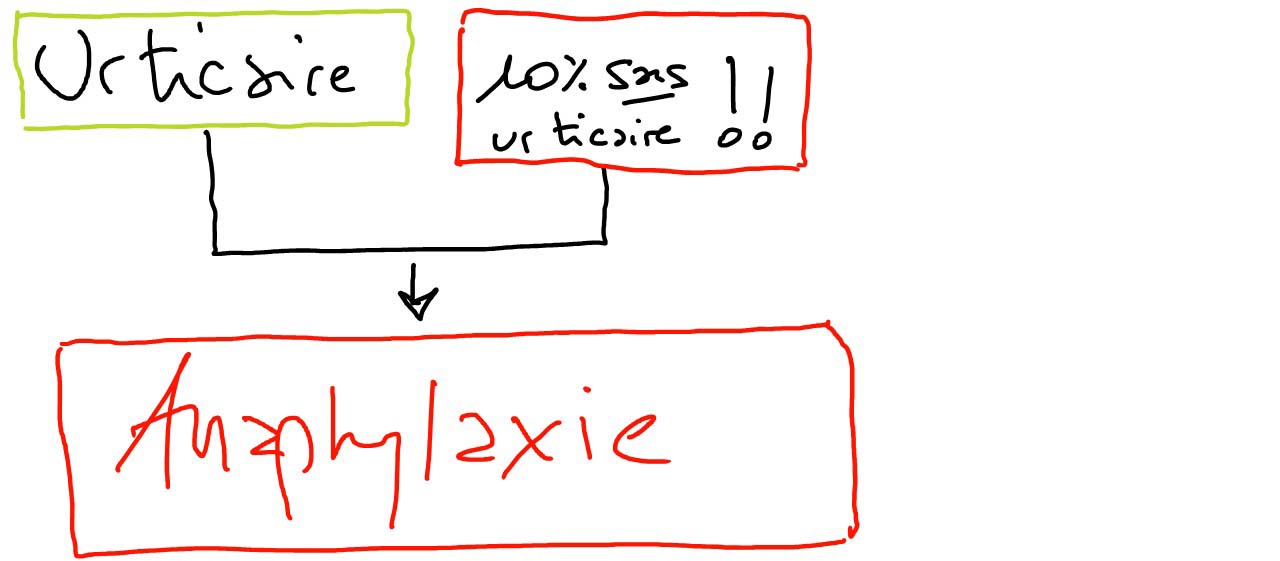
sinon IM A répéter facilement:

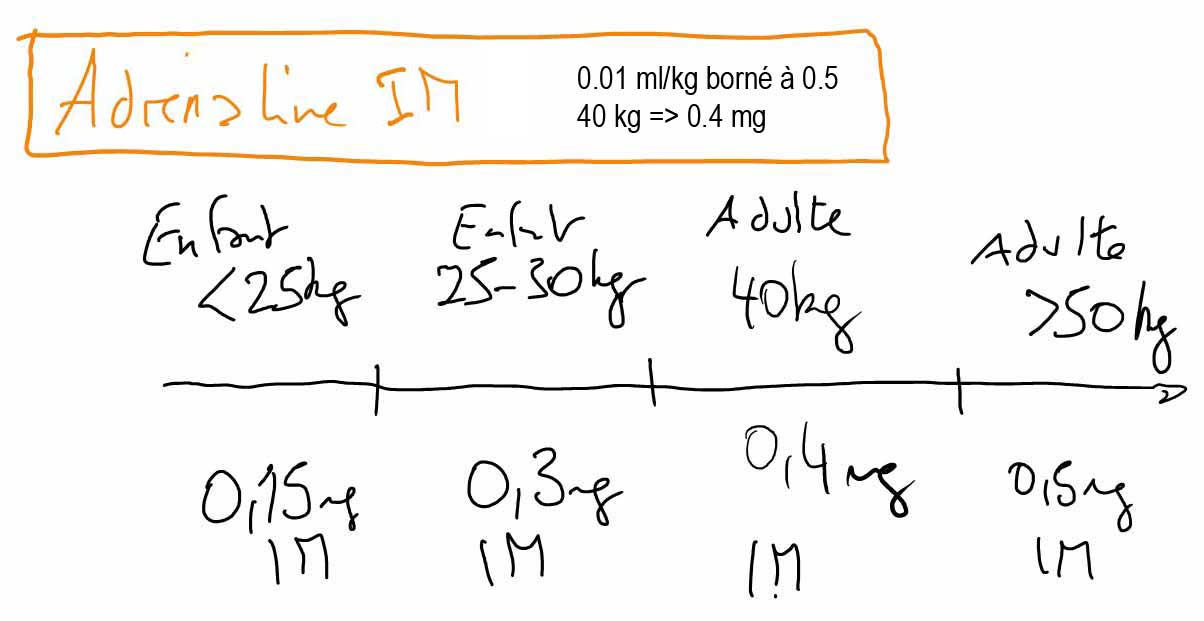
IM face antéro-externe de la cuisse en 10 secondes:
Puis
En paralléle: ATT: Les antihistaminiques et corticoïdes réduisent les symptômes mais ne traitent pas l'anaphylaxie: ils ne doivent pas retarder l'injection! [Lancet]
!!! Revoir les posos ici: [RFE anaphylaxie SFMU 2016]
[Urgences-serveur.fr] "En raison du risque d’arythmie létale souvent secondaire à une erreur de posologie, la voie IVD devrait être réservée au risque imminent d’ACR, aux formes réfractaires, ou devant une instabilité hémodynamique sévère chez un patient déjà perfusé." [SFMU 2016]
En cas de traitement par bêta bloquants : augmenter la posologie de l’adrénaline, si inefficacité de l’adrénaline : Glucagon 1à 2 mg IVD à renouveler toutes les 5 min.
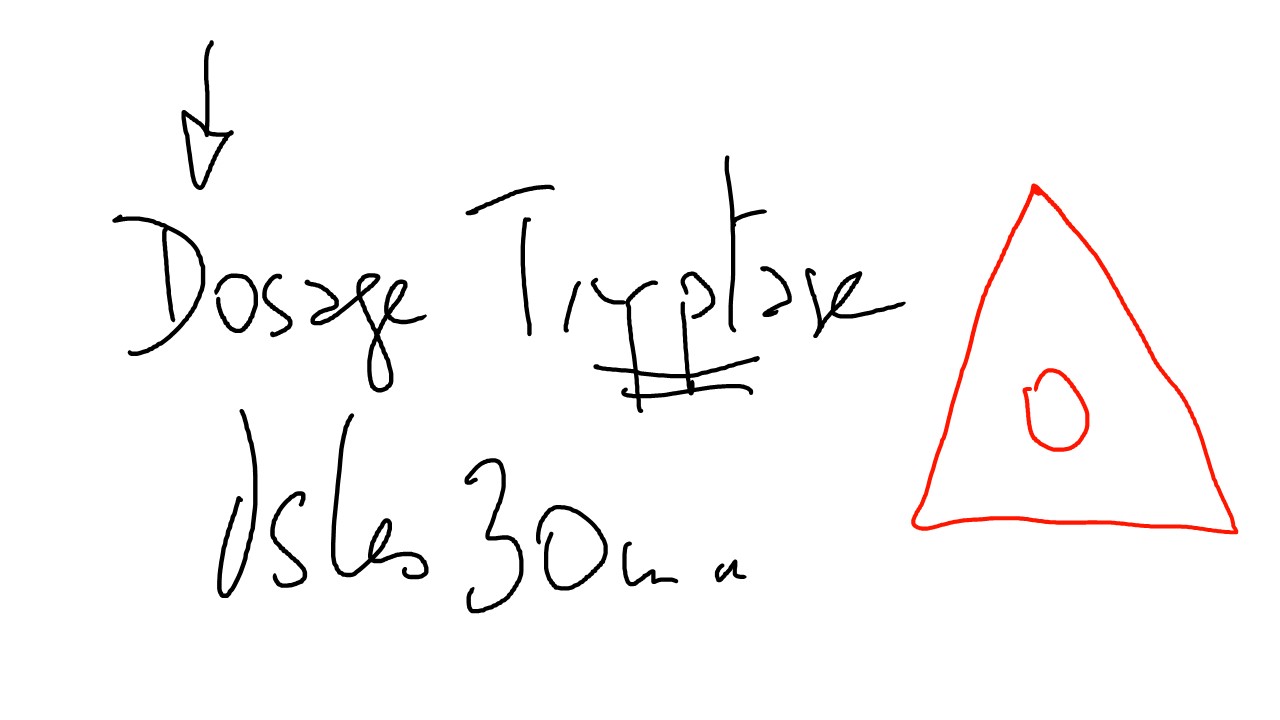
3 prélèvements: à l'arrivée (idéalement à 30mn), H2 et H24: dosage de l'HISTAMINE, TRYPTASE, IgE Spécifique
Le dosage de la tryptase sérique a amélioré les possibilités de dépistage de la mastocytose, qui doit être évoquée systématiquement en cas de réaction anaphylactique sévère ou de manifestation trainantes: avoir le dosage facile.
5% had biphasic reactions. Biphasic reactions were more common where hypotension was present at initial reaction. The median time to onset of biphasic symptoms was 11 (range 0.2–72) hours, that is, 50% of reactions occurred >11 hours after initial reaction. Steroid administration did not affect the likelihood of a late phase reaction.
Patients over 16 years are observed for 6–12 hours after anaphylaxis (children under 16 should be admitted). [Mythes 2019]
Cf. RFE anaphylaxie SFMU 2016 en annexe
Myth 1: ‘Anaphylaxis often results in death’ fatal anaphylaxis is (fortunately) a rare event. Severe anaphylaxis, however, is unpredictable, Therefore, it is critical that all anaphylaxis reactions are treated as a medical emergency. Fatal (and in our experience, near-fatal) anaphylaxis reactions often present as acute bronchoconstriction without any other symptoms being present.
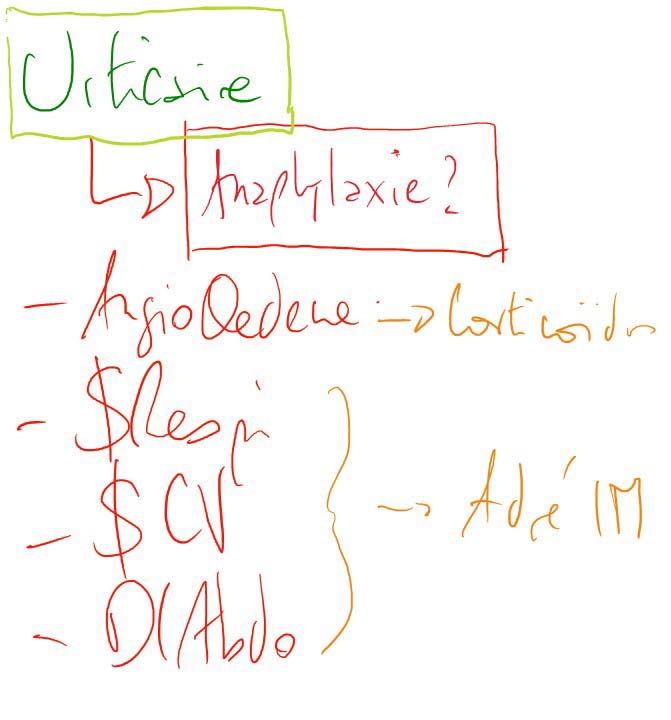
Myth 2: ‘There are no hives so it can’t be anaphylaxis’ Cutaneous symptoms (most commonly urticaria or ‘hives’) are absent in around 10% of anaphylaxis reactions and where present may be delayed in onset.
Myth 3: ‘No trigger for the reaction is identified, therefore it is not anaphylaxis’ The most common trigger in young people is food: symptoms typically begin within 15–30 min of exposure and progress rapidly. The most common food trigger for fatal anaphylaxis in children in the UK is milk, followed by peanut and tree nuts. Other triggers, such as medication or insect stings, are far less common in children. In around 20% of cases, no trigger is identified. Therefore, always consider anaphylaxis in someone with a known food allergy who has sudden breathing difficulty.
Myth 4: ‘Epinephrine is dangerous’ Epinephrine is the first-line treatment for anaphylaxis according to all guidelines. Epinephrine given by intramuscular injection into the outer mid-thigh is very safe and starts to work within minutes. Epinephrine can and should be repeated after 5 min; the administration of other medication such as antihistamines or steroids must not cause delay or distraction, as these are not first-line (or even second-line) treatments for anaphylaxis
Myth 5: ‘Antihistamines can be used to treat anaphylaxis initially; epinephrine is only needed if symptoms worsen’ Antihistamines are not effective against anaphylaxis: their prophylactic use does not prevent anaphylaxis. their use is limited to the relief of cutaneous symptoms
Myth 6: ‘Corticosteroids prevent delayed or biphasic reactions in anaphylaxis’ Steroid administration did not affect the likelihood of a late phase reaction
Myth 7: ‘Only children who have had anaphylaxis need an epinephrine autoinjector’ Myth 8: ‘Epinephrine autoinjectors are overprescribed and overused in anaphylaxis’ Myth 9: ‘Prescription of an epinephrine autoinjector in isolation is life-saving’
Patients and their families need to be told to use their autoinjector in the event of any respiratory symptoms, where anaphylaxis might the cause, irrespective of severity.
PEC version [RFE anaphylaxie SFMU 2016]
PEC version GHT Normandie Centre: